Wednesday
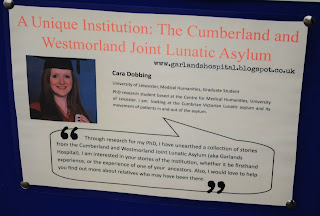
8th November saw the launch of our exciting project surrounding the
Garlands Asylum. Along with Cumbria County Council, Cumbria Partnership Trust,
and Carlisle Eden Mind, I presented some of my research, which focused on the
history of this fascinating institution. The aim of the project is to break
down the stigma surrounding mental health by opening up the discussion around
the treatment, as it was in the early days of the asylum, and as it stands now,
and the help people can access in the event of mental illness. The value of
reflection lies within the lessons we can learn from the progression in
terminology, treatment and the way we consider mental health. Through this post
I will outline the main points I made at the launch, and hope you will join the
discussion surrounding mental health.
My
focus, of course, is on the history of the Garlands Asylum, and how mental
conditions were treated in the period from its opening in 1862, until the
outbreak of war in 1914. Placing the patients’ stories and experiences at the
heart of my research has caused me to regard the institution with a human aspect.
When people ask about my research, and I mention the phrase ‘lunatic asylum’,
they have a large misconception about the brutality of treatment received, and
regard the institution with a degree of horror. Through my research I aim to
breakdown these misconceptions and retell its history through the patients who
experienced treatment in the institution.
My
talk began with giving a short background of the asylum: when it was
constructed, why, what kind of treatments were offered, and the effect this had
on the patients. I then set out the regime of care from the inception of the
asylum in 1862, and continued throughout the initial decades.
Moral Treatment
Moral
treatment, was advocated in all county asylums in the period after 1845. The main facets of this regime were not
dissimilar to some of the recommended treatments today: a good diet, regular
exercise, recreational activities, religion and useful employment. This
treatment was outlined in the 1863 Garlands annual report by the medical
superintendent, Dr Clouston:
To treat the patients kindly, to maintain good order and discipline in
the house, to provide healthy and suitable employments for all who can employ
themselves, to endeavour to get those to work who do not do so, to provide
suitable entertainments for their leisure hours, to endeavour to get them all
roused into taking an interest in something, thus exercising and strengthening
the mental faculties they have left, and to keep up the bodily health and
strength in all of them.
He placed great emphasis on the employment of the
patients to act as a diversion from the thoughts and circumstances causing
their conditions: regular work for both
mind and body will do much to counteract the ill effects of the associations of
the persons, places, and circumstances that were connected with the original
outbreak of the malady.
Around
three quarters of the asylum population were regularly employed. Tasks in the
workshops, on the farm, and in the asylum itself were largely carried out by
the patients. The result was noted in the 1869 annual report as ‘pleasing and
amusing’ the patients to a great extent.
Patients, that were able, were allowed to walk in
the asylum grounds, with supervision from the asylum attendants, in order to
get regular exercise. This was said to have had a soothing effect on the
patient’s behaviour as they got the opportunity to clear their thoughts in the
fresh air. Similar to this were the recreational pursuits offered to the
patients to keep them usefully occupied whilst in the asylum. A large supply of
books and periodicals were available. Knitting, needlework, domestic chores,
work on the asylum farm, were all undertaken by the patients to encourage
productivity and recovery, as well as contributing to the upkeep of the asylum.
Regular events would be held to keep the patients occupied. Weekly dances and
balls would be held. Sports events, such as cricket, would occur, with teams
being brought in to compete with the patients. Choral groups, ventriloquists,
and lecturers would be invited in to the asylum to give performances.
Patients who were otherwise unruly could respond
well to these events. For instance, Catherine B, who was admitted in February
1885 suffering with mania and suicidal tendencies, seemed to forget all this
and react well to the asylum dances. As described in her case notes in April
1885:
Wanders about the ward moaning and groaning wretchedly. The only occasion
in which she appears to forget her troubles is at the weekly dance, when she
brightens up wonderfully. Laughs heartily and industriously goes round the
hall... Labouring hard often to teach others the steps and educate her fellow
patients who require it.
There are many instances of patients responding well
to the moral regime of the asylum. This was noted in the 1887 annual report: the disinclination many patients have shown
to leave the asylum, shows that the efforts made to treat the inmates justly
and kindly, and to render their life here pleasant and enjoyable, have been successful.
For
more background on Moral Treatment, see my previous post - http://garlandshospital.blogspot.co.uk/2015/09/the-moral-treatment-of-patients.html
Misconceptions
The main focus on my talk was to break down some of
the common misconceptions of the Asylum. These are the main three I have come
across. First: once patients were admitted, they were incarcerated for life. Overcrowding
of the asylum, and the pressure on accommodation in the institution was a
constant problem. As early as 1863, one year after opening, the Committee
of Visitors stated of Garlands: ‘they are
unable to provide sufficient accommodation therein for the number of lunatics
who are chargeable to the two counties.’ The asylum underwent several
extensions in its initial decades, taking the available capacity from 200 in
1862, to 660 patients in 1902. Taking this into account, the unnecessary
incarceration of patients simply was not feasible. Doctors were driven by
statistics, and were judged on their rates of recovery. So when a patient came
to the asylum, they did their utmost to affect a quick recovery, to maintain a
high rate of cure. As we saw in the Garlands recovery rates, they managed to do
this. Therefore, it was in the doctor’s interests to keep the patients for as
little time as possible in order to free up any available beds, and so that
they maintained their professional reputation among the relatively new field of
psychiatry. How well this quick-turnaround actually worked is doubtful, as many
patients were readmitted to the asylum at a later date, often in a worse
condition than when they were first treated.
The second biggest myth is that the patients were
subjected to frequent brutality. The common belief is that asylums kept
patients constantly in chains or strait jackets. However, as I have shown
previous, the regime of moral treatment completely disregarded this practice.
Patients were treated with kindness and given the opportunity to adhere to the
moral therapy offered. When patients rebelled against this kindness, the
doctors only sought to use methods of restraint as a last resort. Violent
patients would firstly be placed in a single room on their own and given the
opportunity to calm down: Sedatives would also be administered. If the violence
continued, and they posed a risk to themselves or others, methods of restraint
would be sought. All patients who were placed in mechanical restraints had to
be recorded in a specific register, and this would be inspected by the lunacy
commissioners on their annual visits.
For instance, in 1891, it was recorded that eleven
patients had been put in seclusion for a total of 257 hours across the whole
year, and that one man had been restrained for 8 hours using sheets, and one
woman using the strait jacket for 15 hours, across the whole year. Therefore,
although mechanical restraint was used, it was only done so as a last resort,
and was not the common mode of treatment.
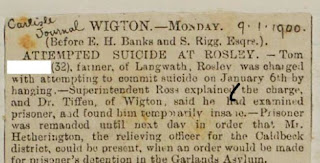
The last biggest myth is that patients, in
particular females, were admitted to the asylum against their will and without
suffering from mental illness. I often get people asking me if there are lots
of women put in there because they annoyed their husbands and such, but so far
I have found no evidence of this. I think that this practice may have occurred
in earlier decades and centuries among the wealthier classes who could afford
to pay doctors to take their wives into private asylums. But Garlands was a
public asylum that provided treatment for pauper patients, and was paid for by
local Poor Law Unions. The 1845 Lunacy Act stated that to be admitted to a
county asylum, the testimonies of two individuals that had witnessed the
person’s insanity had to be recorded on a document called a reception order.
These testimonies had to come from an examination from a doctor or medical
officer at the local workhouse, and from a relative/neighbour/fellow workhouse
inmate who had lived closely with the patient. The form then had to be signed
by a local magistrate warranting the person’s removal to an asylum. There are
instances of paper work being filled out incorrectly and patients being
discharged as a result. Therefore the method of entry to an asylum was much
more rigid than many people believe.
Next Steps
From the discussions began at the launch, it is
clear that more is required to really address the stigma surrounding mental
health. By using the past as a way of reflecting on how much (or how little)
treatments have changed, we hope to continue debating what is required in
future to treat mental illness.
The exhibition of the some of the Garlands archival
materials will be shown at several venues around the county. Full details and dates
will be confirmed shortly, and we hope as many of you as possible will be able
to view it.
For full information of the launch see
Any feedback of the event, and any comments you may
have for suggestions of where we could take the project, please don’t hesitate
to get in touch. Caradobbing@gmail.com